What is Ovarian Cancer?
Ovarian cancer is a disease in which, depending on the type and stage of the disease, malignant (cancerous) cells are found inside, near, or on the outer layer of the ovaries. An ovary is one of two small, almond-shaped organs located on each side of the uterus that store eggs, or germ cells, and produce female hormones estrogen and progesterone
Ovarian Risk Factors…
- All women are at risk
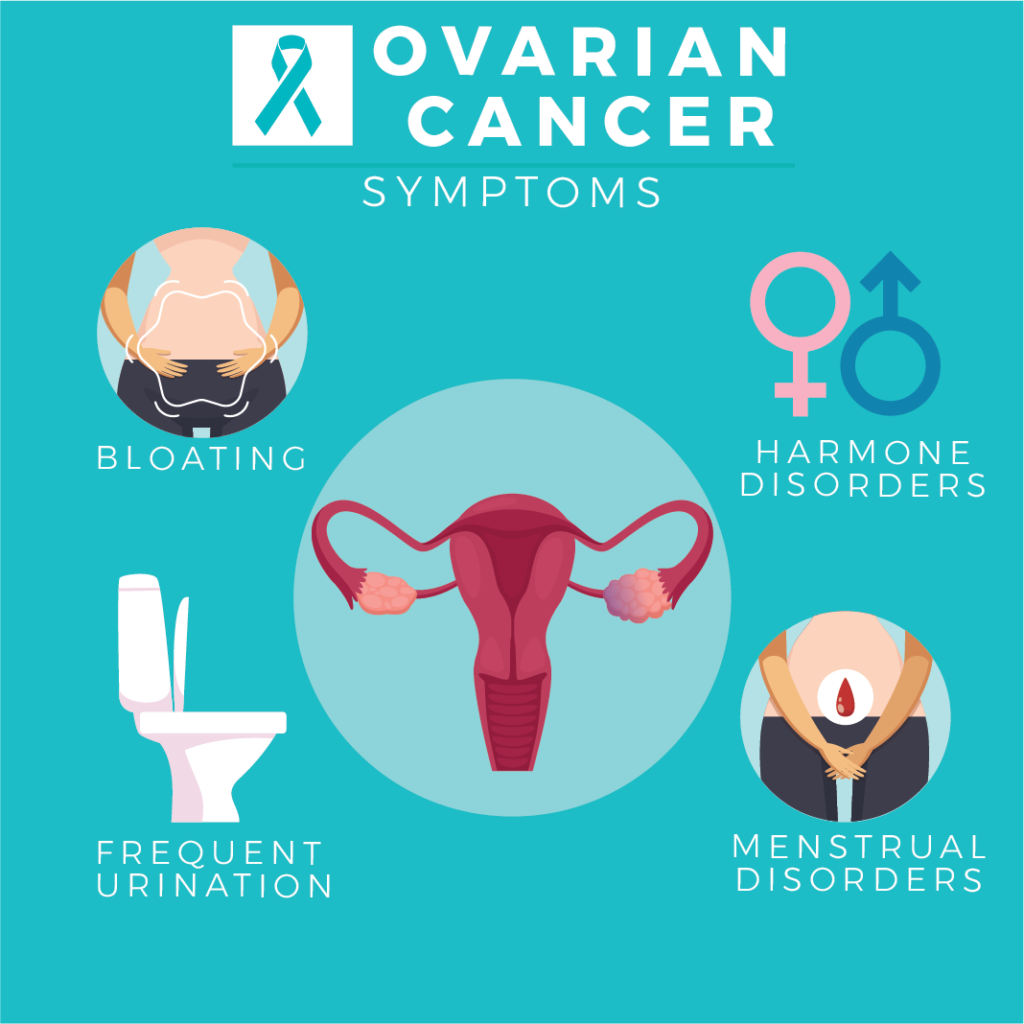
- Symptoms exist – they can be vague, but usually get more intense over time
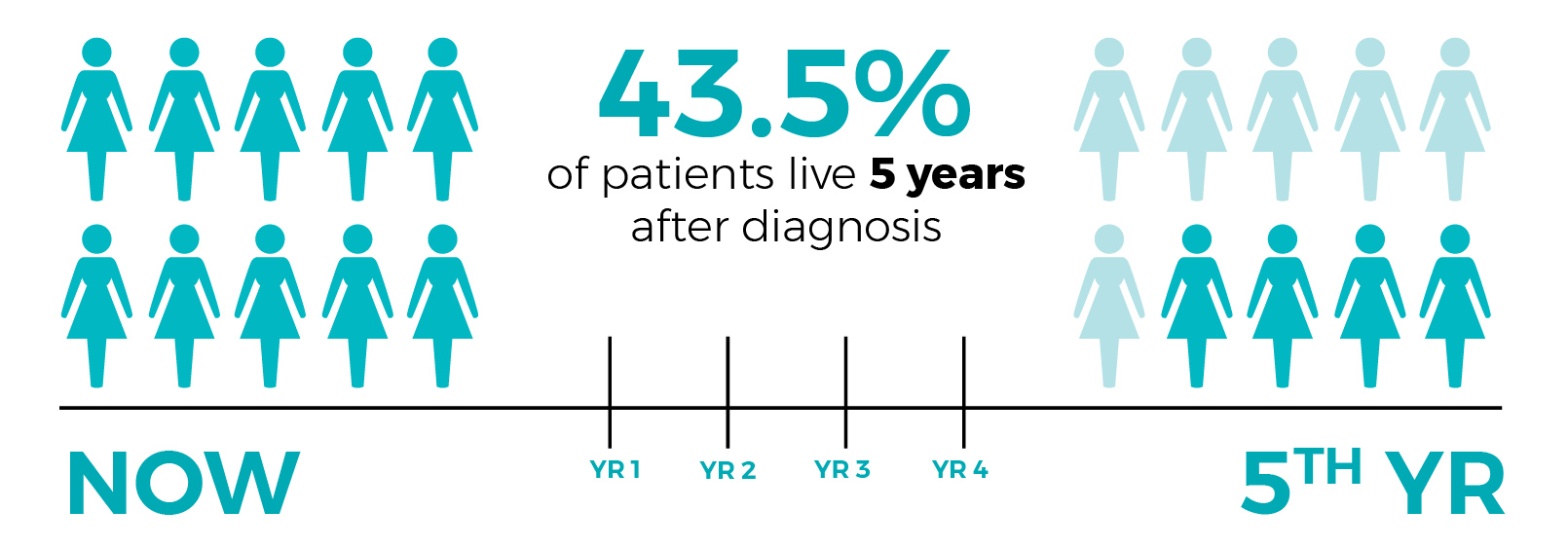
- Early detection increases survival rate
- A Pap test DOES NOT detect ovarian cancer
Ovarian cancer risk factors include:
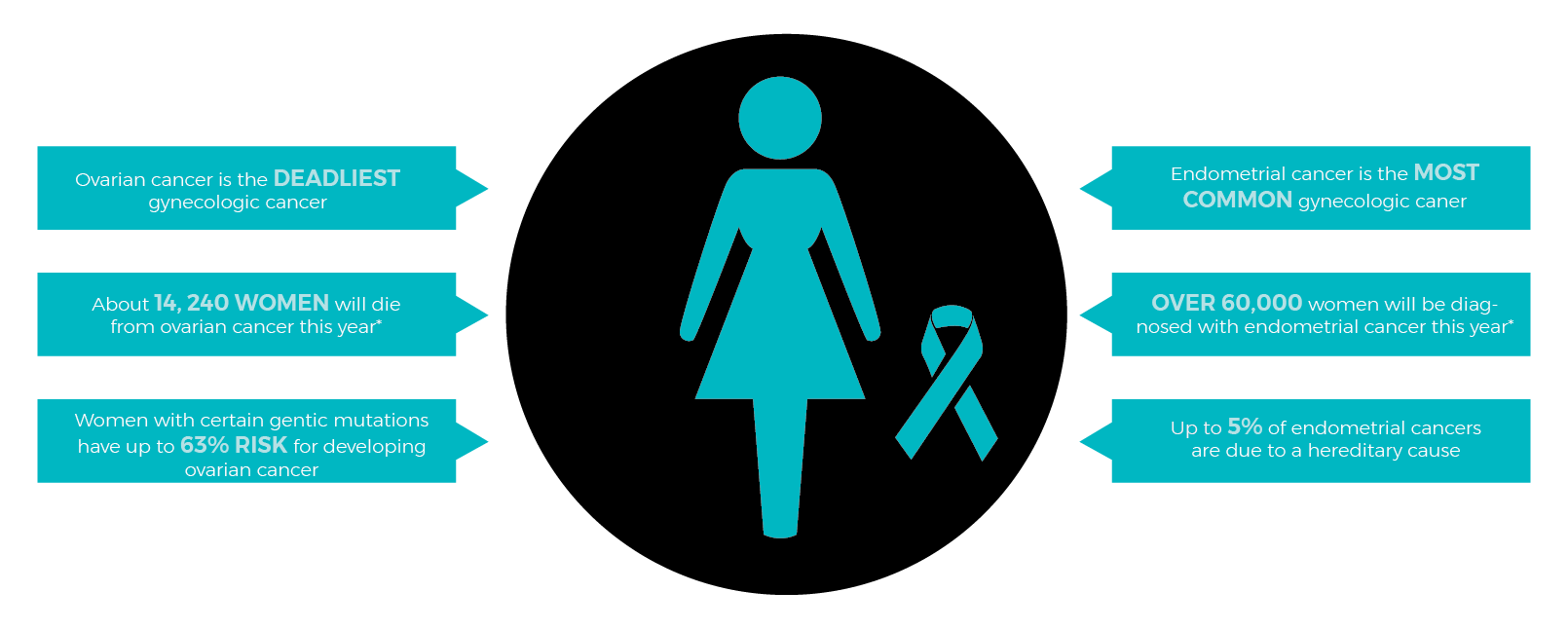
- Genetic predisposition
- Personal or family history of breast, ovarian, or colon cancer
- Increasing age
- Infertility
While the presence of one or more risk factors may increase a woman’s chance of developing ovarian cancer, it does not necessarily mean that she will get the disease. A woman with one or more risk factors should be extra vigilant in watching for early symptoms.
Recommendations
Current recommendations for management of women at high risk for ovarian cancer are summarized below:
- Women who appear to be at high risk for ovarian cancer should undergo genetic counseling and, if the risk appears to be substantial, may be offered genetic testing for BRCA1 and BRCA2.
- Women who wish to preserve their reproductive capacity can undergo screening by transvaginal ultrasonography every six months, although the efficacy of this approach is not clearly established.
- Oral contraceptives should be recommended to young women before they embark on a planned family.
- Women who do not wish to maintain their fertility, or who have completed their family, may undergo prophylactic bilateral salpingo-oophorectomy. The risk should be clearly documented, preferably established by BRCA1 and BRCA2 testing, before surgery. These women should be counseled that this operation does not offer absolute protection because peritoneal carcinomas occasionally can occur after bilateral oophorectomy.
- Since BRCA1 and BRCA2 gene mutations also increase the risk of developing breast cancer, annual mammography screening is suggested, beginning at age 25.
- Women with a documented HNPCC Syndrome, also known as Lynch Syndrome, should undergo periodic screening mammography, colonoscopy, and endometrial biopsy.
For more information: www.ovarian.org